Building Confidence when Discussing Treatment Cost
Jul 13, 2023
It is possible that in caring too much we may sabotage our treatment outcomes.
If you're someone who feels uncomfortable discussing treatment costs with your clients, you may be inadvertently impacting the quality of care you provide.
By getting more comfortable with discussing uncomfortable topics, we are able to improve the quality of our care.
I say this as someone who genuinely wishes I could work for free, because I wish that there was 100% equity in healthcare, that the best care wasn't available to only those with deeper pockets.
I say this as someone who, after noticing at times I was potentially negatively impacting my client's perceptions of what may have been their best course of care, because I was making assumptions about their position in relation to the cost of the treatment intervention(s), I paid to have my ass kicked by various mentors, coaches and other professionals over the years to address this mindset, because I was aware I needed a shift, but didn't know where to start.
Often what makes us great clinicians, our empathy, compassion and genuine want to help others, can be the very same thing that undermines our ability to deliver the best possible care.
I do recognise that we all work in vastly different locations, all with their own unique cultural and socio-economic demographics. So whilst there won't ever be one piece of advice or insight that will apply to everyone, I do hope that this article provides some strategies that may help if you are someone who is guilty of feeling guilty.
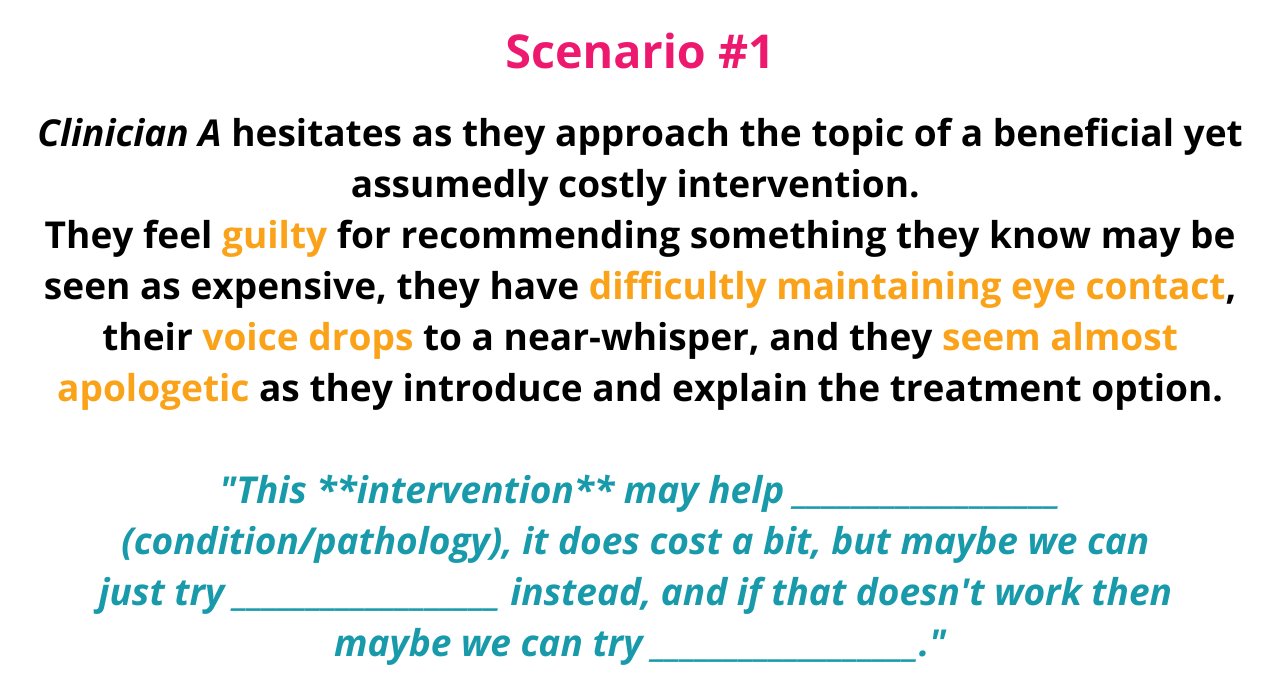
Due to the demeanour and delivery of this information from Clinician A, this lack of confidence may lead to the patient perceiving the recommendation as less credible or not important.
They may sense the clinician's discomfort, leading them to now feel uneasy and doubtful about the treatment as well.
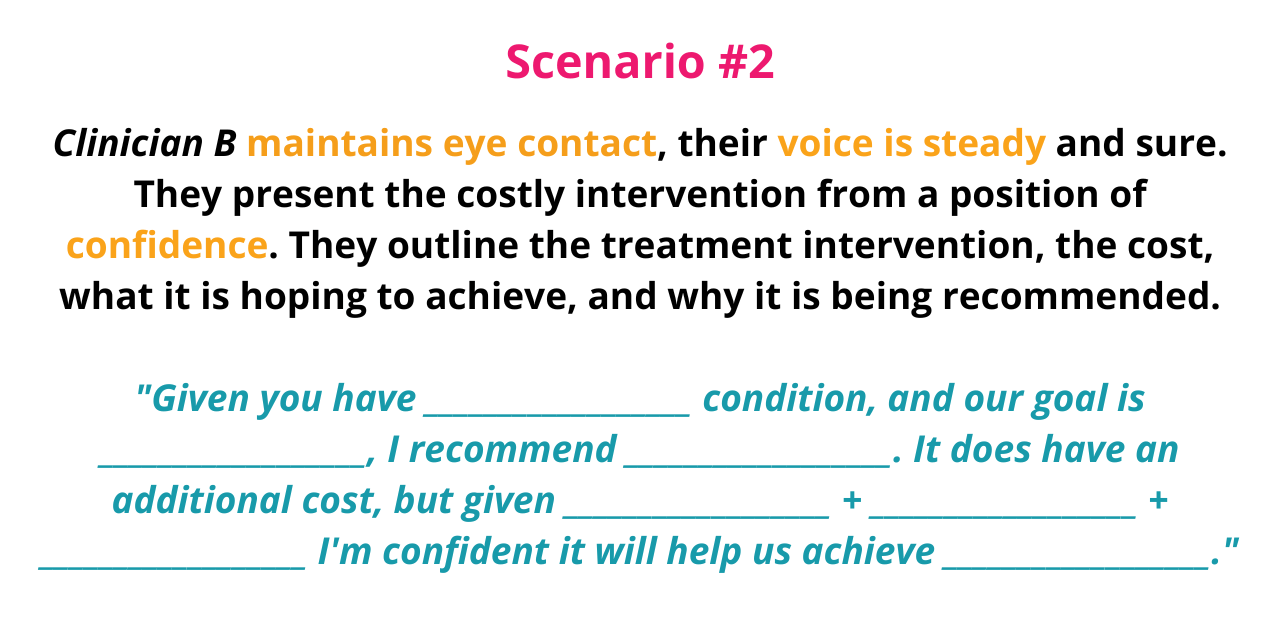
Clinician B, even if they are caring & compassionate, has not let the cost of the treatment affect their confidence in making the recommendation.
The confidence & straightforward approach, the clear explanation and linking the client's goals to the therapeutic goal gives the patient the opportunity to understand why the treatment is being recommended, despite the additional cost.
As humans there are a lot of behavioural elements we perceive without knowing we are, language, demeanour etc. we observe all of it and respond accordingly, even if we're not aware that we are.
It is this element that I want to focus on today...
The Double-Edged Sword
When it comes to our roles as health practitioners, our primary goal is to deliver quality, ethical care, that promotes the health and well-being of our patients. Our recommendations are grounded in evidence-informed practice and driven by the desire to facilitate achieving optimal health outcomes.
However, many of the things that make us great at our jobs - empathy, compassion, a sense of social justice, can actually be the very things that detract from delivering the best care possible.
The unease we experience when having conversations regarding additional &/or out-of-pocket expenses can inadvertently shape our demeanour, subsequently altering patient perceptions, and ultimately, impact the care we are able to deliver.

Guilt can be one of the primary emotions that drives this lack of confidence, rooted in the assumption that patients may not be in a financial position to afford the extra cost of the proposed treatment.
We may worry that by recommending this treatment intervention that we may be causing financial stress or appear 'salesy', veering away from our role as providers of healthcare.
These fears, while they may be well-intentioned, are often based on our own projections rather than the actual financial capacity of our patients.
Admittedly, I am not an expert in consumer behaviour and psychology.
However, I have found that by deferring to others for their guidance and addressing my own belies and behaviours on this topic, it has made be a more confident clinician, providing better care.
Am I Guilty of Projecting?
Here are a few questions that you can ask yourself and reflect on, to give you an idea of if this is something you may be doing.
1. How often do I avoid discussing higher-cost treatments due to concern about a patient's financial status? Do I leave it up to my administration staff to discuss price?
If it is frequent, you might be making assumptions about your patient's financial capacity.
2. Do I feel uncomfortable or anxious when discussing treatments with higher costs even before the topic has been raised with my patient?
If you answered yes, the discomfort may stem from your assumptions.
3. Do I find myself making judgements about a patient's ability to afford treatments based on their appearance, background or referral method (eg: EPC)?
If you answered yes, this may be a clear sign that assumptions may be impacting your treatment recommendations.
4. Do I feel relief when a patient declines a higher-cost treatment option?
If you answered yes, you may have been allowing your preconceptions and own beliefs impact your treatment discussions.
5. Do I assume patients would rather opt for a less effective but more affordable treatment?
The assumption can impact what treatment options you may be presenting, and also how you're presenting them.
6. Am I transparent about all available treatment options regardless of cost?
If not, you may be presuming what your patients can/can't afford.
Whilst there certainly will be situations where price sensitivity comes into play during our clinical practice, it pays to reflect on our ongoing patterns and beliefs
The Impact on Quality Care
It is no secret that perception and expectation can grealty influence outcomes.
If we demonstrate hesitancy and/or a lack of confidence, we can be inadvertently compromising the quality of care that we provide.
Our discomfort, demonstrated by our body language and demenour, can impact the interactions with our patients, potentially reducing their trust in our expertise and recommendations.
Further to this, our behaviour may negatively influence a patient's perception and potential efficacy of a treatment option, or we may even be limiting their treatment options, all from a well-intentioned place of potentially proritising cost considerations over healthcare outcomes.
As healthcare providers, our confidence matters.
It influences how our patients perceive us, their acceptance of our advice, and ultimately their health outcomes (read more here).
Building Confidence
The first step to mindset or behaviour change is sel-awareness.
Earlier in the article we asked ourselves some questions to identify if we may be allowing out assumptions and preconceptions impact how we are bringing ourselves to the interaction, ie: are we price sensitive.
Now we'll explore some strategies to overcome price sensitivity if it is impacting our clinical practice and patient care.
Detatchment
Remember, you're treating your patient not their wallet! (thank you Tom - I stole that from you).
Also, you're not deciding for the patient, you're providing them with options.
You're giving them enough quality information about the role of the treatment intervention relating to their pathology, their goals and the therapeutic effect the interventions will aim to provide, then you're outlining associated costs.
If after discussing treatments and costs there may be further discussions on navigating affordibility.
Whilst this may seem like basic b*tch advice, regularly reminding yourself of this is one of the biggest ways to begin shifting your mindset.
If you were in the patient's position, would you want to be provided with all available options and price OR have the information being shared with you curtailed based on the clinician making an assumption about your financial position?
Provide Options
In the context of podiatric practice, orthoses and footwear are often the two most expensive treatment interventions we may discuss, especially when we are recommending the two combined.
New shoes plus orthoses can head upwards of $700, even more depending on your clinic's location and pricing.
When I owned my clinic, it was in a region of lower to mid-socioecomic status.
As a resut, I would offer payment plans for custom and pre-fabricated foot orthoses.
The pros were that it often removed or at least lessened the financial barrier for a number of my clients.
The cons were that it ran the risk of me being out-of-pocket.
I would however, take a deposit before sending off the orthoses scans or dispensing the pre-fabricated devices, at the least it would often cover the cost should the client fail to pay.
Did I get burned? Yes.
I would say out of 7 years I can recall 2 instances where a client failed to pay off the remaining balance. Bad debt isn't ideal, bills need to get paid, but I didn't lose sleep over it (having a good policy & procedure around your financial options, as well as being discerning with who, what and when the options are discussed greatly helps in this regard).
There were possibly 5 or 6 instances beyond this where clients were not paying their instalments. However, a letter outlining that per the contract signed failing to settle the remaining balances would result in the matter being referred to a debt collection agency, this got things back on track almost instantly.
Would I offer payment options again if I opened another clinic? Yes.
Whilst it is annoying having your income impacted by clients doing the wrong thing, or having to chase-up outstanding payments, the amount of people who it benefited and helped me navigate the complex emotions I felt.
There are other financial services that you can engage who handle this for you.
For the cost of the services versus the cost of the therapeutic interventions that I was providing payment plans for, I chose to bear the risk myself.
If you are concerned about your patients' ability to afford certain therapeutic interentions, it may be worthwhile having payment plans available, but weight up the pros and cons carefully.
Focus on Communication
Be transparent and compassionate when discussing costs, but work on staying neutral in your body language and demanour (remember, it does impact perceptions).
Clearly explain the role of the therapeutic intervention (ie: clearly link the client's goal(s) to your therapeutic goals - more here).
By fostering clear communication, inviting questions and nagivating the treatment options with your client, this is shared decision-making in practice, and this is what leads to quality care.
Whilst there is no definitive fix to address the complex emotions we may feel as clinicians looking to help our patients as much as possible, by shifting how we look at the situation of cost vs care, and recognising that by providing our patients with all the information from a place of neutrality we are actually improving the quality of our care.
As always, I hope I have been able to provide some insights and strategies to help you in your healthcare journey.
I you've found this content helpful the best way to say thanks is to share this with your progressively-minded colleagues.
Join the Research Round-Up
Free monthly newsletter, delivering the latest research straight to your inbox
Research Round-Up delivered at the end of each month

