Delivering Impactful Education without Creating Overwhelm
Jun 02, 2023
It's no secret that education underpins many of the successful therapeutic outcomes we achieve. Yet it can be a fine line to walk, with information overload and heightened patient anxiety or fear being on the flipside of this coin.
How can we provide information to our clients in a digestible and unthreatening manner to keep us on the positive side of the coin?
Background
Best-Practice & Clinical Guidelines now consistently recognise that education is always a first-line treatment option, that contributes to the core management approach for managing musculoskeletal pathologies.
However, what we communicate, when we communicate & how we communicate needs to be tailored to the individual.
The Importance of Client Education
Client education is crucial in our management for a number of reasons.
Firstly, recognising that knowledge is power.

When someone is given the opportunity to understand their condition, their body and what they can do to help themselves, it allows them to become active participants in their healthcare journey. By providing them with the knowledge and tools they need to make informed decisions about their treatment options.
Secondly, there are also numerous bodies of work that consistently demonstrate that effective patient education can improve treatment engagement & adherence, often leading to improved treatment outcomes and overall patient satisfaction.
Limitations in Information Retention
While the significance of effective patient education is clear, it's important to recognise that there are limitations to our memories and cognitive load (the amount of information one can hold at a time).
The Cognitive Load Theory, developed by educational psychologist John Sweller in the 1980s, suggests that our working memory can handle only a limited amount of information at any given time. Providing patients with too much information can lead to confusion, misunderstanding, forgetfulness of important details and even heightened levels of anxiety & fear.
Insights & Strategies Towards Better Client Education
There are a few tips & strategies that can assist us in improving what & how we communicate often complex information to our clients.
Tailoring Communication to the Client
Understanding your patient's level of health literacy is an important first-step. Health literacy is "the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand and use information in ways which promote and maintain good health." - World Health Organisation.
Those with a lower level of health literacy may struggle with medical jargon and complex explanations (word salads don't belong in healthcare!!!).
As health professionals it is important to ensure we are promoting equity in health, and this is an example of how we can do this at an individual level. It is our responsibility to ensure that we are helping our patients understand their conditions, regardless of their prior knowledge or educational background.
Having an understanding of these elements can allow further tailoring your education to your client:
- Health literacy - this can be explored simply from listening to how they communicate elements of their clinical and other health history. The words they use, how they explain things when you ask for more information etc...
- Social & occupational background
- Previous treatment experiences - how they explain what was done, why it was done (if known) and what the effect was.
Communicating Complex Information Simply
This is a skill that takes time and practice to develop.
Conveying complex medical information in simple, relatable terms is a skill that every healthcare professional should continually develop.
Using metaphors, analogies, real-life examples, or everyday language can be an incredibly useful strategy to help make complex concepts more understandable.

In addition to the words we speak, we need to recognise that not everyone is an auditory learner. Using visual aids and patient-friendly educational resources can significantly enhance their comprehension and understanding.
One of the best papers that outlines this is Lived experience and attitudes of people with plantar heel pain: a qualitative exploration - (read it here).
This is one paper I discuss in-depth across a number of the P3 courses, because it gives us some really insightful, actionable recommendations to help improve our client education and the overall client experience.
Actionable Steps to Improve Educational Communication
Keep it Simple
Try to break down complex information into simple, digestible chunks.
This takes practice! Using analogies and examples can really help.
Remember, word salads don't belong in healthcare!
An example I use regarding tissues and how they respond to movement.
Case Example: Let's say I have a patient with Achilles Tendinopathy and they're wanting to understand why things feel stiff and sore initially, then it "warms up" or it's a relatively inactive person who feels stiff and sore from not moving, which the initial stiffness and discomfort discourages them from moving more.
Analogy: Rusty gears and grease.
"Picture you have 2 rusty gears with no grease, trying to move them will take more effort and isn't as efficient.
But then we apply some grease and then start to move the gears. It's easier & they move better. This is what movement does, the grease are all the good things in our body that help our tissues stay healthy or heal if they're injured.
In our bodies what creates the 'grease' is movement.
So we need to move frequently and intensely enough to make the grease - too little activity or too much activity isn't good.
Let's say we stop for too long, the grease dries up, then we're back to the start. Or if we have grease, but move the gears for too long or too fast - this can cause friction and stop the gears working efficiently too."
Communicating: "Motion is lotion" - movement promotes fluid flow in & out of tissues, which is required for tissue healing, tissue adaptation & maintenance of tissue health.
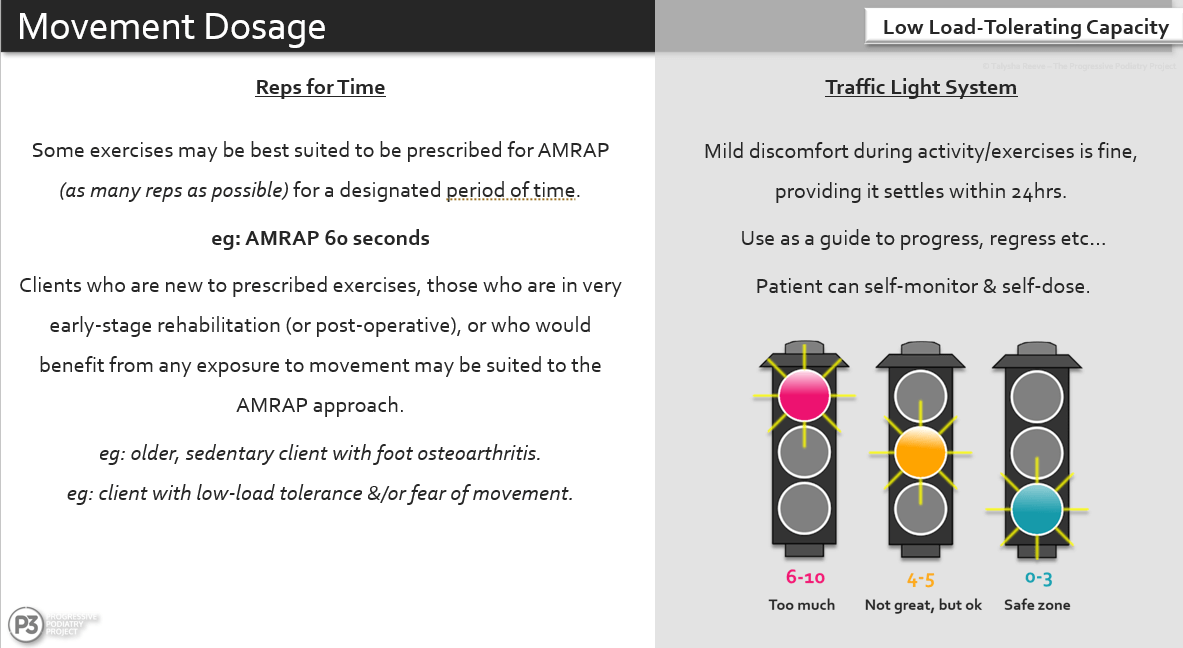
This will usually be built upon with a load management plan, or an exercise &/or movement prescription that uses the Traffic Light System to self-dose the prescribed activities (aka AMRAP VAS-P - As Many Reps As Possible in-line with the Visual Analog Scale of Pain).
Whilst no analogy is perfect and there's certainly some people who it doesn't work with (that's why we just keep learning different ones to find a repertoire to draw from), I find it helps get people understanding the importance of frequent, dose-appropriate movement for their healing & long-term health.
For those unfamiliar with the Traffic Light System and VAS-P - here's a slide from some of the online courses & workshops I run, where we discuss rehabilitation dosage.
Use Visual Aids
Diagrams, charts, models, whiteboards and other visual tools can help enhance understanding, especially for our visual learners.
I am a huge fan of using a whiteboard and using this whilst I am explaining something to a client. This can be from structural changes in tendinopathy, load-recovery cycles for tendon loading, stages of bone stress injuries - you name it, I like to draw it (or at least try!).
Check & Reflect
Regularly check-in with your patient to see if they understand what you're explaining.
What I tend to do after we've covered some educational aspects is say; "Ok, so let's pretend that when you get home you need to explain what we've just covered to your wife/husband/housemate etc, what would you tell them?"
This gives the opportunity for information consolidation for them, but also gives us an opportunity to clarify any pieces that may have been missed or misunderstood.
Promote Open Communication
People often shy away from asking questions to clarify. Whether it's in a patient consultation or in an educational workshop, not everyone will let you know if they aren't understanding what you're saying.
Sometimes we have to take the lead and encourage our patients to ask questions and voice any concerns they have.
Not to mention an open dialogue will foster trust, aid in understanding and give us even more insights into who we are working with - allowing further tailoring of our communication & treatments.
Overall, the key is individualisation. The more we learn, the more we communicate and the more we collaborate with our clients, the better we can individualise and help them get the most out of our care.
Hopefully this articles gives you some insights into where we may be able to refine our communication and education, to improve our client outcomes.
Join the Research Round-Up
Free monthly newsletter, delivering the latest research straight to your inbox
Research Round-Up delivered at the end of each month