Plantar Fascioptahy vs Fasciitis vs Fasciosis
May 13, 2025
Author: Talysha Reeve | B.App.Sc.(Podiatry), GradCertClinRehab
WORDS MATTER
If you're diagnosing patients with plantar fasciitis and have found that the treatments you've provided haven't worked (or made things worse!) this article will help you understand some reasons why.

In clinical practice, we will often try to explain complex medical information to our patients in simple terms. However, there are times when attempting to simplify this information sets us (and our patients) down a misdirected treatment path.
The purpose of this article is to;
a) Provide you with a nuanced understanding of the importance of utilising correct terminology when describing plantar fasciopathy.
b) Provide you with a resource that you may direct your clients to, to help them understand why some treatments may or may not have been effective for the treatment of their condition.
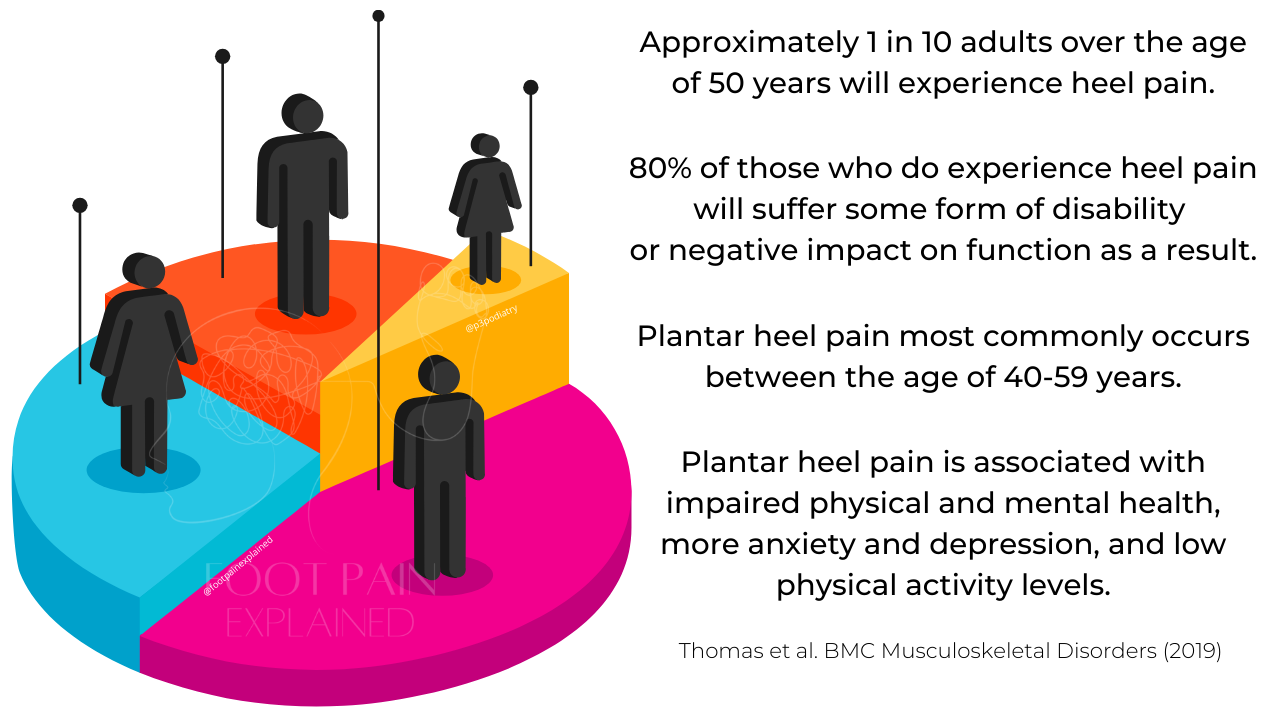
Plantar heel pain is incredibly common, with research consistently reporting up to 1 in 10 adults will experience this in their lifetime.(1)
Given the exceptionally high lifetime prevalence and the multitude of driving factors that contribute to the development of this condition, it stands to reason why treatment responses vary considerably between individuals.
One of the keys to understanding why some treatments are more effective for different people lies in the name itself - fasciitis.
What we will be covering in this article: the difference between plantar fasciitis, fasciosis and fasciopathy.
What we won't be covering in this article (but will in others): the in-depth nuance of plantar heel pain, all of the elements that factor into the condition, the various treatments for plantar heel pain and their effectiveness.
The plantar fascia is a thick band of connective tissue that originates at the heel and connects to multiple structures at the forefoot.
↓
"Aponeurosis is a sheath-like connective tissue that aids in force transmission from muscle to tendon and can be found throughout the musculoskeletal system".(7)
What is an Aponeurosis?
Firstly, it is not a tendon or a ligament!
An aponeurosis is a sheath-like, fibrous connective tissue structure found within many muscle–tendon units.(7)
It acts as an intermediary that transmits force from the contractile elements of muscle to the passive tendon or directly to bone or adjacent soft tissues.(7)
Aponeuroses are typically collagen-rich and highly anisotropic, meaning their mechanical properties differ depending on direction, which aids in force distribution and energy transfer within the muscle–tendon complex.(7)
Names Commonly Used as a Diagnosis for Plantar Heel Pain
Over the years, plantar heel pain has been diagnosed in a number of ways, including:
- Policeman’s heel
- Jogger’s heel
- Subcalcaneal pain
- Plantar fasciitis
- Plantar fasciopathy
- Plantar fasciosis
- Heel spur syndrome
Despite almost all of the conditions listed above affecting the plantar fascia, some nuance exists between many of the conditions.
Each of these "conditions" affecting the plantar fascia typically have their own characteristics, can involve other structures, have variations in the sub-groups of people they're more likely to develop in, and will often vary in what factors may contribute to developing the condition in the first place.
Diving into the variations between conditions is beyond the scope of what we're discussing today, but the most important take-away so far is;
One condition/pathology can have numerous variations in cause, clinical presentation and appropriate treatments between individuals.
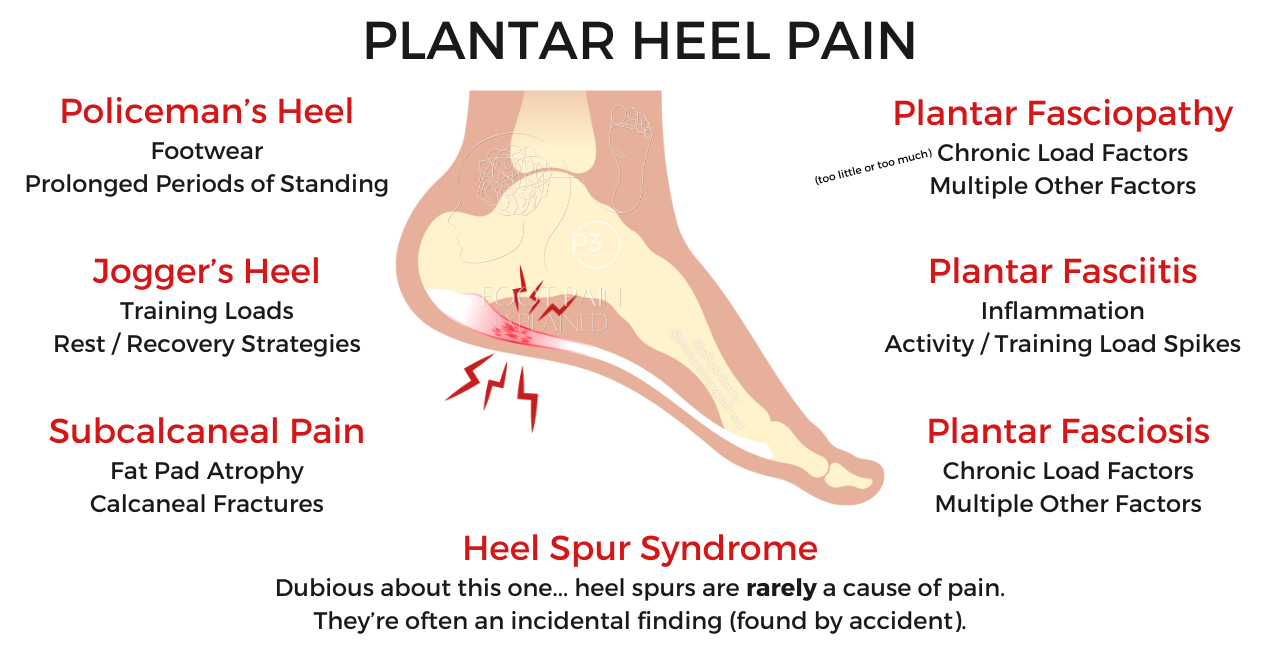
Whilst often used synonymously, these terms describe somewhat different conditions.
Plantar Fasciitis ≠ Heel Spur Syndrome ≠ Plantar Fasciopathy
Words Matter
Unfortunately many health professionals and some researchers are still utilising plantar fasciitis as the "one-size-fits-all" diagnosis for plantar heel pain, despite a multitude of research publications determining that fasciitis is not the most appropriate term. Whilst the diagnosis of plantar heel pain is considered more appropriate, due to the condition frequently affecting other tissues in the region.
Today, we're focused on understanding the key differences between plantarfasci- ‘-itis’, ‘-osis’, and ‘-opathy’.

What Is Plantar Fasciitis?
Plantar fasciitis is often used to describe heel pain associated with inflammation of the plantar fascia—a thick band of tissue connecting your heel to your toes.
The term implies an inflammatory process is at play (indicated by the suffix “-itis”).
However, research suggests that true inflammation is not always present. Instead, long-standing cases often show signs of degeneration and/or disorganisation of the connective tissue that forms the fascia, not inflammation.(2, 3, 4, 6)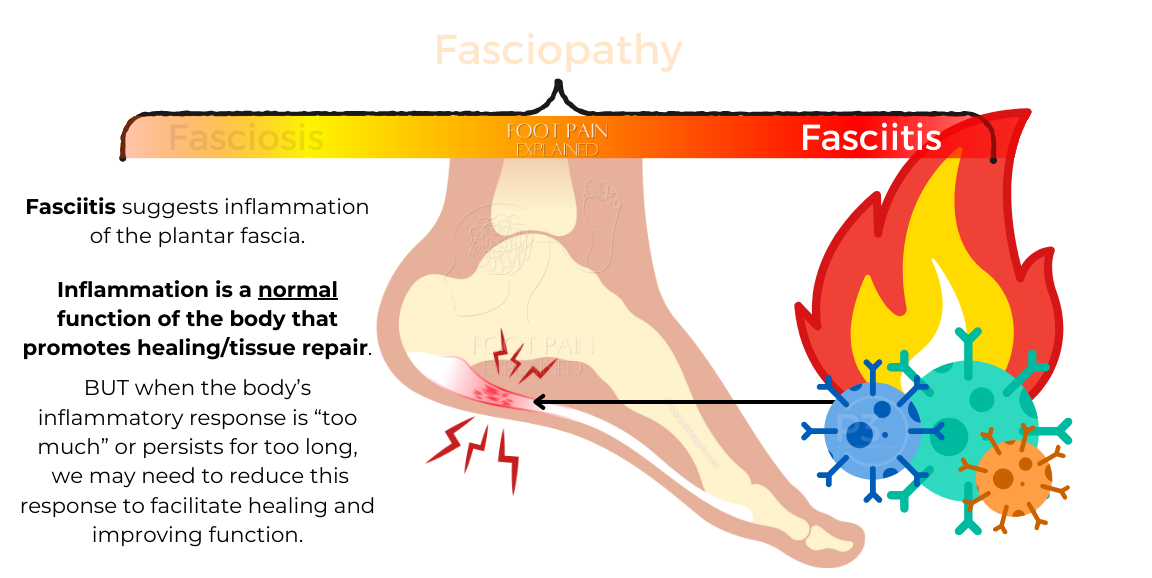
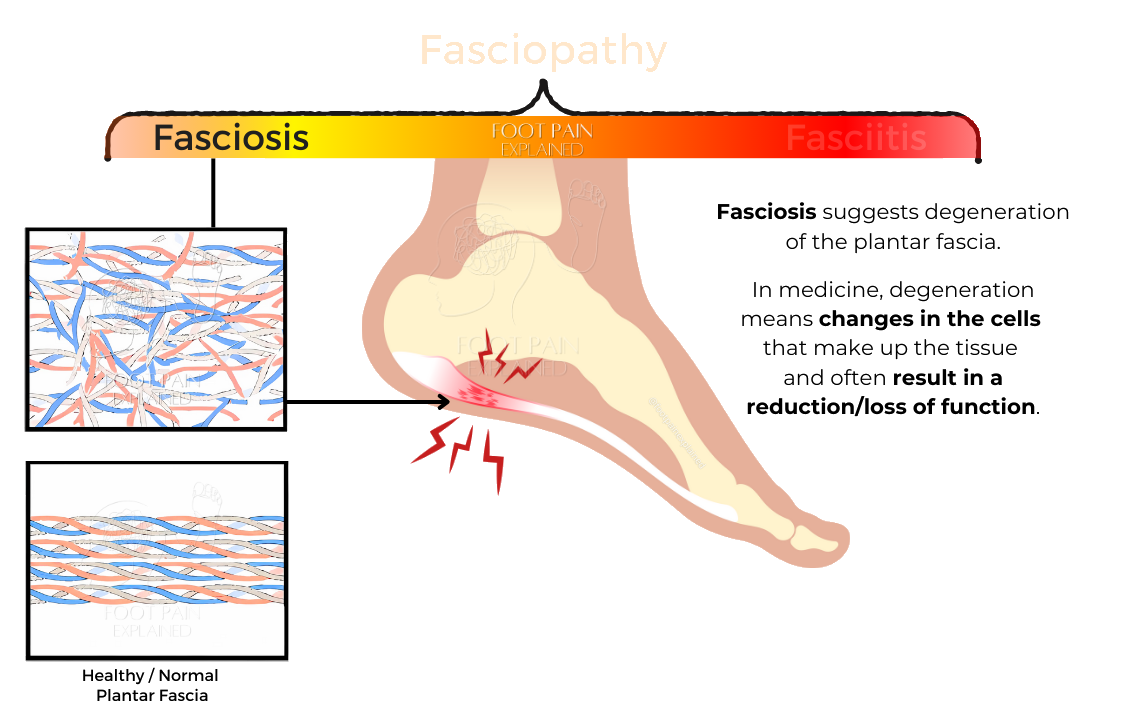
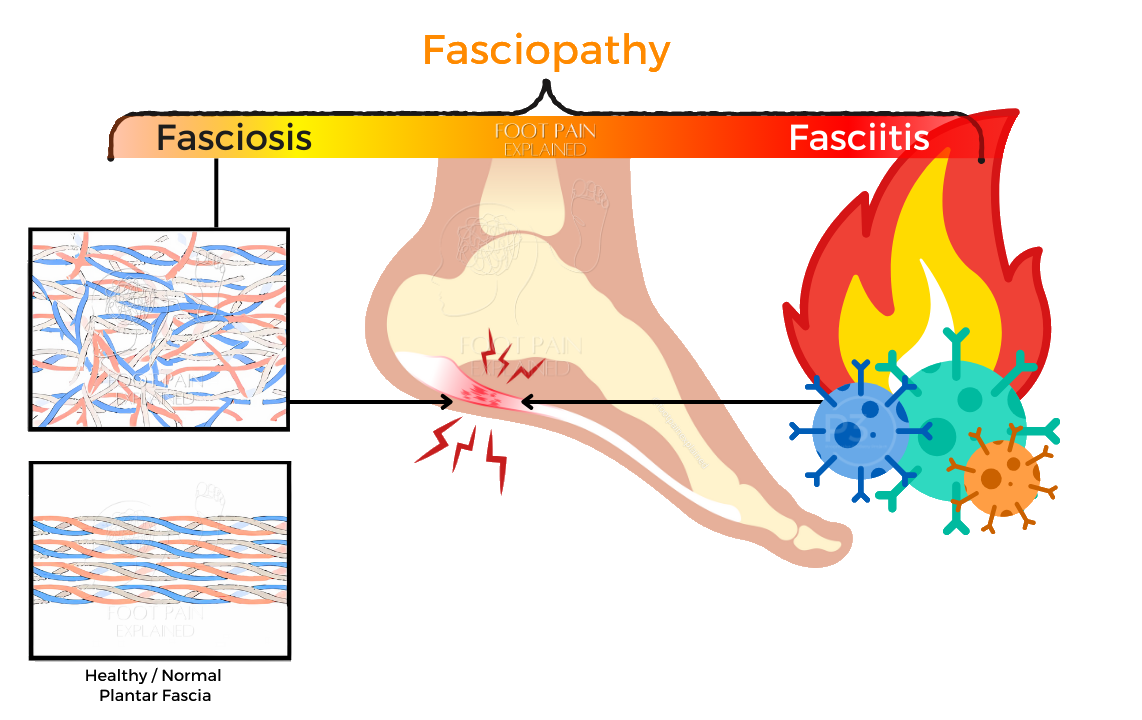
What Is Plantar Fasciosis?
Plantar fasciosis refers to a degenerative condition of the plantar fascia.
It’s characterised by structural changes to the plantar fascia, without the signs of inflammation typically associated with “-itis” conditions.(2, 3, 4, 6
This means treatments aimed at reducing inflammation might not always address the underlying cause of pain and/or impaired function.
What Is Plantar Fasciopathy?
Plantar fasciopathy is a broader term that encompasses both the inflammatory and degenerative changes that may occur in the plantar fascia.
Why Does the Terminology Matter?
Using the right terminology helps:
Understand the condition: Knowing whether your heel pain involves inflammation and/or degeneration influences treatment decisions.
Set realistic expectations: If structural changes (fasciosis) are the primary driving factor of symptoms and functional impairment, appropriate treatments and recovery may vary and take longer than conditions purely driven by inflammation.
Improve communication: Consistent terms reduce confusion between clinicians and patients, improving clinical decision-making.
Key Differences Between ‘-itis,’ ‘-osis,’ and ‘-opathy’
“-itis” (Plantar fasciitis): Suggests inflammation.
“-osis” (Plantar fasciosis): Refers to degeneration without inflammation.
“-opathy” (Plantar fasciopathy): Covers a spectrum of conditions, including inflammation and degeneration.
Where things can get confusing for both patients and health practitioners managing plantar fasciopathy, is that people presenting with the condition may have differences in the main "driver" of symptoms.
For one person, inflammation may be the primary factor contributing to pain.
For someone else, their pain may be driven more as a result of load intolerance; pain in response to certain intensities or durations of movement/exercise.
That is, the body or area experiences pain almost as a "warning" that its telling you that it feels like the load being applied is too much (more nuance to this will be unpacked another time).
For others, they may have both structural changes ('-osis') and inflammation ('-itis') presenting at the same time, with one type potentially being more dominant.
This is exactly why fasciopathy is a more accurate and appropriate term.
This image below illustrates how different people may have different "drivers" of their heel pain.
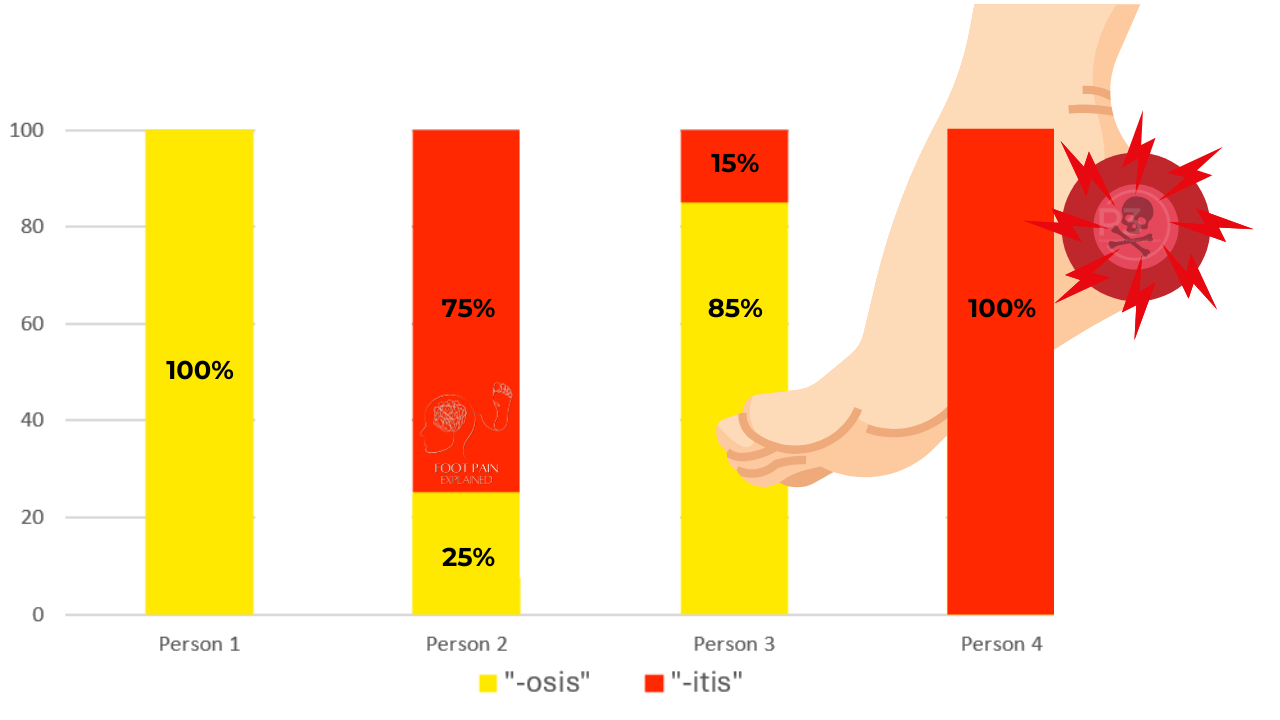
Person 1: 100% fasciosis and 0% fasciitis; changes to the cellular structure of the plantar fascia, making it less load-tolerant.
Person 2: 25% fasciosis and 75% fasciitis; some changes to the physical structure of the plantar fascia can be present, with a relatively high degree of inflammation contributing to their pain.
Person 3: 85% fasciosis and 15% fasciitis; a high amount of structural changes to the plantar fascia and low load-tolerance, with a small amount of inflammation present.
Person 4: 100% fasciitis and 0% fasciosis; an otherwise "healthy" structure that may have been acutely overloaded, resulting in a large inflammatory response.
There certainly is more nuance to this topic, however, for the purpose of keeping this article relatively clear and concise, we'll leave it with this simple delineation between the three terms.
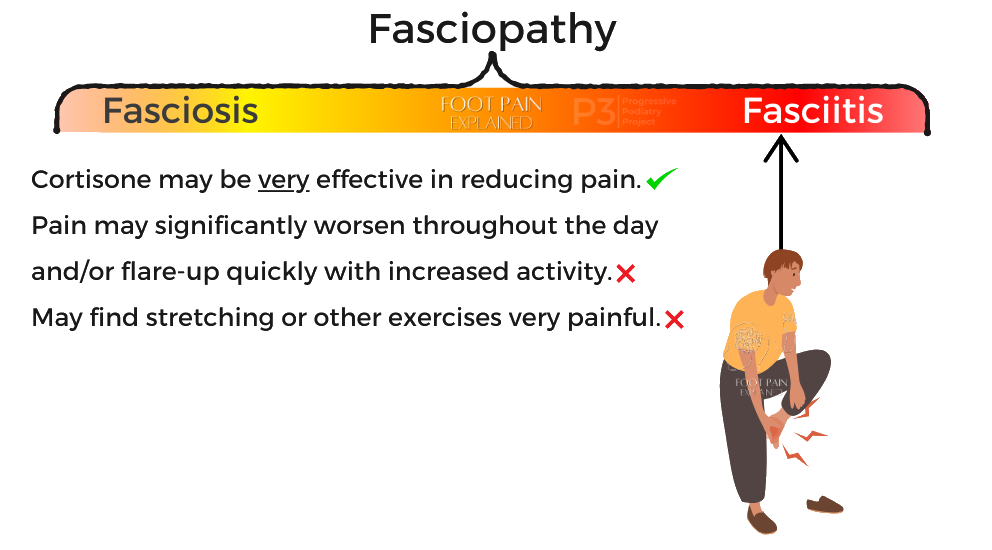
Influence on Treatments with ‘-itis,’ vs ‘-osis,’ vs ‘-opathy’
“-itis” (Plantar fasciitis)
Cortisone injections may be effective in reducing pain, whereas some exercise therapies may aggravate symptoms.
Interventions to reduce load (reduce physical activity, rest, strapping, orthoses, footwear changes etc) may be required.
Rehabilitation exercises may need to be low "dose" to balance helping symptoms and not overloading the already inflamed tissue.
“-osis” (Plantar fasciosis)
Cortisone injections may not be effective in reducing pain, whereas exercise therapies can be highly effective in addressing symptoms.
Interventions to alter load (strapping, orthoses, footwear etc) and build load tolerance (progressively increase exercises and activities) are often the cornerstone of treatment.
Other interventions may also help with symptom management to allow more movement to occur (e.g., shockwave therapy).

“-opathy” (Plantar fasciopathy)
As there may be elements of both inflammation and degeneration present to varying degrees based on the individual, cortisone may (or may not) have some effect, and exercise (or other therapies) may also be effective.
The response to all treatments are often dictated by what is driving the majority of symptoms.
Now, we're not even diving into compressive vs tensile-driven presentations - this is another layer of nuance we'll save for another time (or if you want to learn more about that now, click here)
Where treatment and recovery can become incredibly frustrating, is when a person's symptoms flare.
A flare may be due to a spike in inflammation or the area not being inflamed, but becoming "cranky" or less tolerant to movement.
This may look like what treatment(s) were helping before may stop being effective or may feel like they are making the pain worse.
Or a person may find that the pain pattern or what activities they can/can't do change.
Whilst not ideal, flares are quite common. When a pain or/and inflammatory flare occurs, it often means that an individual's treatment plan may need to change to address the variations or fluctuations in the condition.
Key Take-Aways
Heel pain can have many causes and it is not always related to inflammation of the plantar fascia.
Understanding the difference between '-itis', '-osis' and '-opathy' is important (despite what many healthcare professionals say🤬)
There are many instances where heel pain may not be related to the plantar fascia at all!
This will be explored more in-depth in other articles.
If you’re experiencing persistent heel pain that has not responded to treatment or its response to treatment has changed, consult a healthcare professional (or a different healthcare professional) who can assess your symptoms and recommend evidence-based treatments.
Stay tuned for more articles that will explore instances where heel pain is not associated with the plantar fascia.
If you have found this information helpful, or if you know anyone who would benefit from reading any of our content, please share our resources with them.
This article is shared on both The Progressive Podiatry Project and Foot Pain Explained platforms.
© Talysha Reeve
References
- Thomas, M.J., Whittle, R., Menz, H.B. et al. Plantar heel pain in middle-aged and older adults: population prevalence, associations with health status and lifestyle factors, and frequency of healthcare use. BMC Musculoskelet Disord 20, 337 (2019). https://doi.org/10.1186/s12891-019-2718-6
- Riel, H., Cotchett, M., Delahunt, E., Rathleff, M. S., Vicenzino, B., Weir, A., & Landorf, K. B. (2017). Is ‘plantar heel pain’ a more appropriate term than ‘plantar fasciitis’? Time to move on. British Journal of Sports Medicine, 51(22), 1576–1577. https://doi.org/10.1136/bjsports-2017-097519
- Landorf KB. Plantar heel pain and plantar fasciitis. BMJ Clin Evid. 2015 Nov 25;2015:1111. PMID: 26609884; PMCID: PMC4661045.
- Lemont, H., Ammirati, K. M., & Usen, N. (2003). Plantar Fasciitis: A Degenerative Process (Fasciosis) Without Inflammation. Journal of the American Podiatric Medical Association, 93(3), 234–237. https://doi.org/10.7547/87507315-93-3-234
-
Beeson, P., 2014. Plantar fasciopathy: Revisiting the risk factors. Foot and Ankle Surgery, 20(3), pp.160-165.
-
Monteagudo M, de Albornoz PM, Gutierrez B, Tabuenca J, Álvarez I. Plantar fasciopathy: A current concepts review. EFORT Open Rev. 2018 Aug 29;3(8):485-493. doi: 10.1302/2058-5241.3.170080. PMID: 30237906; PMCID: PMC6134886.
- Wheatley, B., et al. (2023). Aponeurosis structure-function properties: Evidence of heterogeneity and implications for muscle function. Acta Biomaterialia. Volume 168, 15 September 2023, Pages 298-308
Join the Research Round-Up
Free monthly newsletter, delivering the latest research straight to your inbox
Research Round-Up delivered at the end of each month

