A Clinical Framework for Developing a Working Diagnosis
Mar 04, 2024
At times it can be overwhelming if we are new to clinical practice and/or dealing with an injury that we don't often see.
This overwhelm can sometimes send us down the wrong path when it comes to our working diagnosis, resulting in wasted time, money, and lead to prolonged recovery times, frustration and potentially, a damaged therapeutic relationship.
Today I want to share a basic framework that, at the very least, will help you develop a systematic way to assess a musculoskeletal region to hone your diagnostics.
Diagnostics, the WHAT, HOW & WHY
In developing an accurate working diagnosis we need to answer the following;
What structure(s) are involved?
How did the injury occur?
Why was it injured?
What structure(s) are involved?
In answering this question we need to;
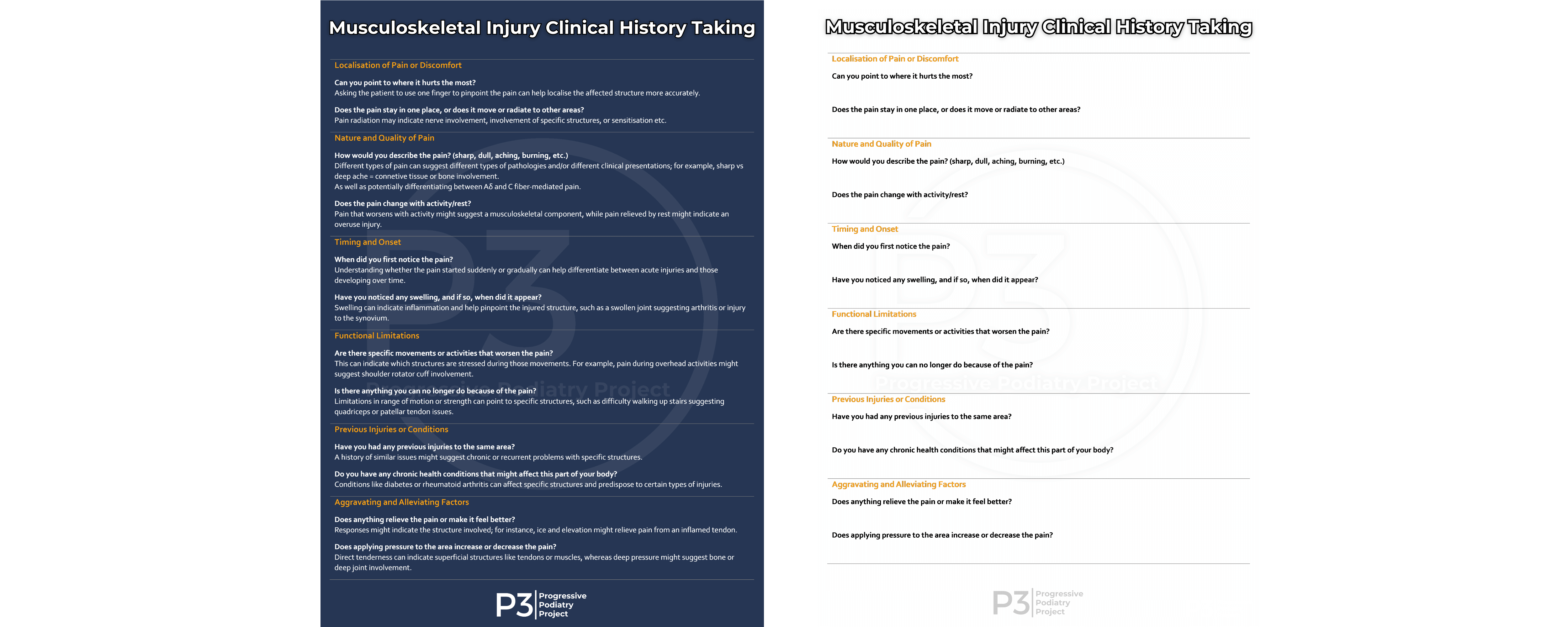
1) Develop our clinical history taking skills.
A thorough history involved exploring the clinical presentation's;
Location, nature, timing, onset, functional limitations, previous injury & health history, aggravating &/or alleviating factors.
Clinical resource for musculoskeletal clinical history taking available via P3 for FREE (here)
2) Have a thorough understanding of anatomy.
Refreshing your anatomy is a key element to developing a reasoned working diagnosis.
Anatomy Framework
Developing a process of consideration for the potentially involved anatomical structures is an effective starting point.
Starting deep & working superficially, or vice versa, works well. Either way, just ensure you consider each structure involved (see below).
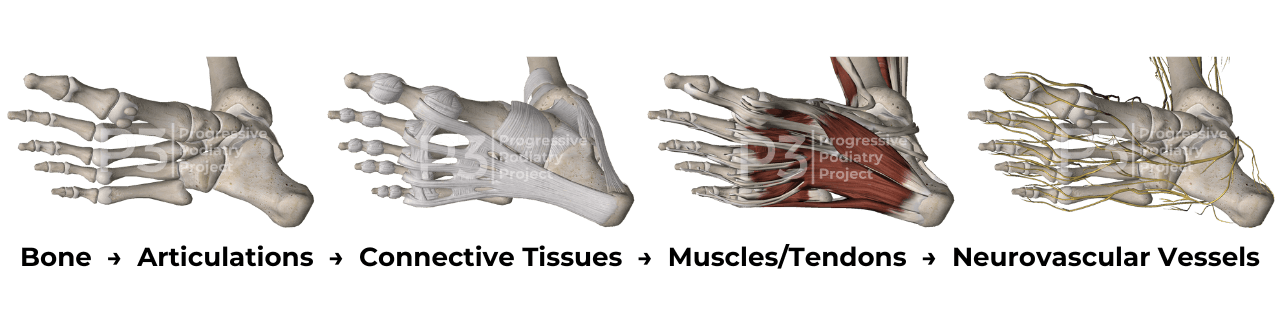
1) What bones are in this area?
2) What articulations do they have?
What joint surfaces are here?
3) What connective tissues cross this region?
Joint capsules, ligaments, bursa, fascia etc...
4) What muscles are in this region?
What tendons insert here?
What muscles/tendons cross here?
5) What neurovasular vessels are in this region?
Nerves, blood vessels & lymphatics.
How did the injury occur?
Mechanisms of Injury
Exploring the mechanism(s) of injury will assist further in honing in on potentially affected structures.
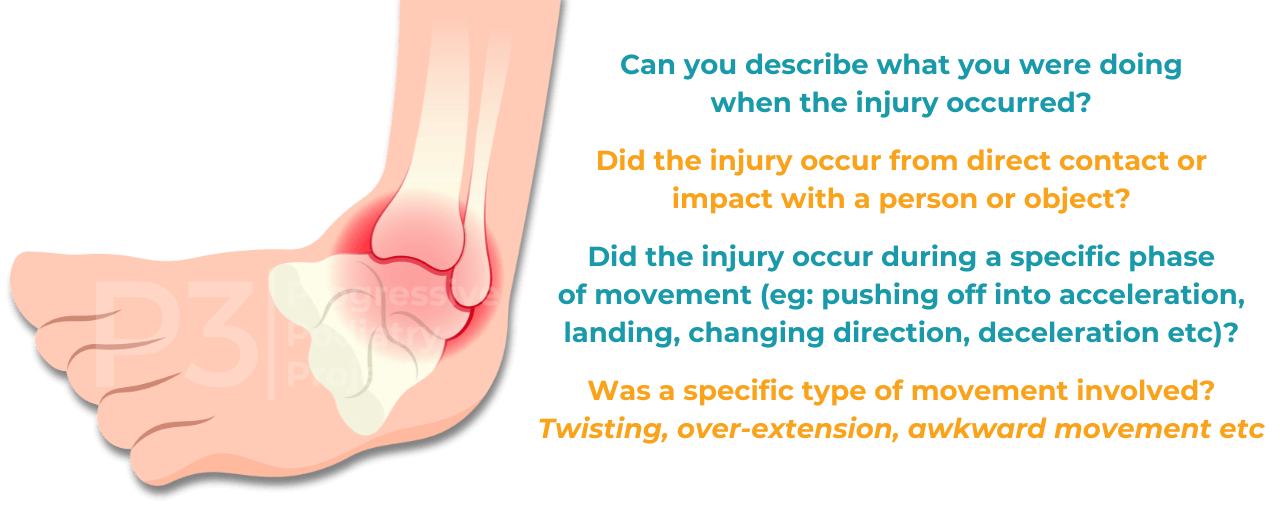
Identifying the mechanism(s) of injury, will help us;
a) Identify if we are dealing with an acute, chronic or flared injury.
b) Gain clarity regarding potential injured tissues.
This becomes important as it will greatly influence the selecting and timing of possible therapeutic interventions.
For example, 3 weeks after an inversion sprain injury to the lateral ankle complex, a patient may present with diffuse hindfoot pain.
Initially you may be thinking the AFTL may be the problematic tissue.
However, upon movement testing (eg: inversion, eversion, dorsiflexion, plantarflexion etc) the patient may report more discomfort around the medial aspect of the hindfoot, suggesting we may need to consider a sustentaculum tali fracture, deltoid ligament injury, injury to the talus &/or articular cartilage.
Expanding on our anatomy framework, when we combine our anatomical knowledge with our understanding of the likely mechanism(s) of injury, we can then move toward a functional anatomy framework for our clinical assessments.
Functional Anatomy in Your Clinical Assessment
Functional anatomy moves beyond the location of a tissue, it also considers how they are loaded in various movements.
When I flex/extend, invert/evert a joint, are the tissues (bones, articular surfaces, connective tissues, muscles/tendons, nerves etc) subject to tensile or compressive loads?
Clinical resource for your Functional Anatomy Assessment available via P3 for FREE (here)
As mentioned previously, a functional anatomy approach to our clinical assessment becomes important, as it greatly influences the selecting and timing of possible therapeutic interventions.
Using the previous ankle sprain example, if we perform our clinical tests and are suspicious of an osseous/articular injury, we may prioritise imaging to rule in/out a more serious injury before implementing a physical rehabilitation program.
Why was it injured?
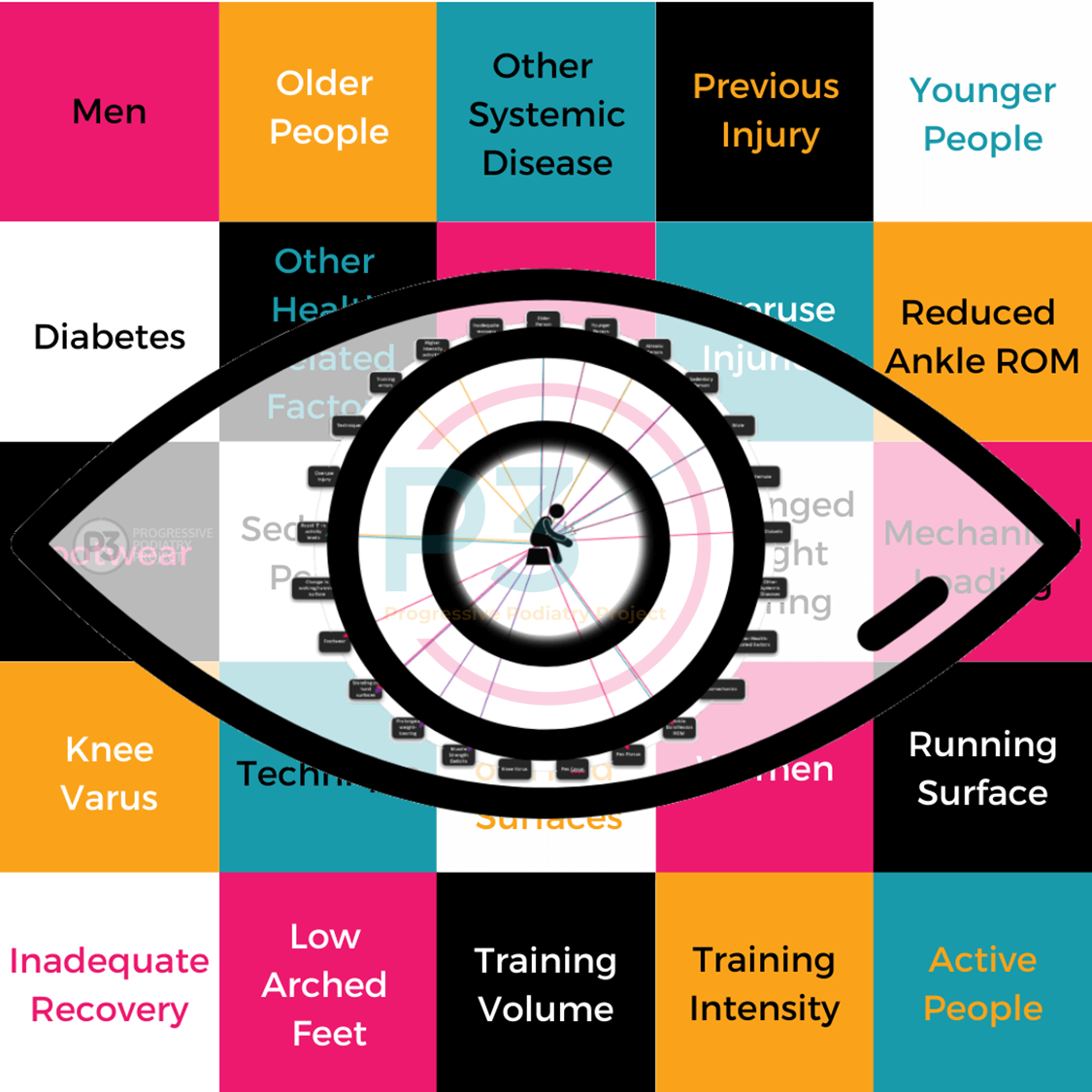
Depending on the type and severity of an injury, we may begin to explore why the injury occurred in the first place during the initial consultation, or later throughout the treatment journey.
The why encompasses the intrinsic and extrinsic risk factors that may have predisposed the person to sustaining the injury. Exploring these factors are essential for developing individualised management plans.
The aetiology of musculoskeletal injuries boil down to a multi-factorial interplay of mechanical load & individual risk factors.
Once we begin to explore the 'whys' of an injury, it becomes easy to understand why no one treatment approach or intervention will work for everyone.
Delving into risk factors extends beyond what we are hoping to achieve today.
I hope this article has given some clarity regarding how we can best approach our initial injury assessments to develop a quick and accurate working diagnosis, so we can get our patients on the right track early on.
Don't forget, you can grab your Musculoskeletal Injury Clinical Assessment Framework clinical resource via P3 for FREE (located in the clinical resources section).
Here are a few other resources that can help you in the next steps of your clinical assessments.
Asking Better Questions Gets Better Results (Blog)
Do You Have Biomechanical Tunnel Vision? (Blog)
Does Every Musculoskeletal Injury Need Rehab? (Podcast)
When LESS is MORE in Rehab (Blog)
Where to Start Plantar Fasciopathy Rehabilitation (YouTube)
Using Tissue Function to Guide Exercise Selection (Blog)
The Art of Therapeutic Goal Setting (Blog)
If you'd like to delve further into assessing and rehabilitation lower extremity musculoskeletal injuries, hit the Explore the Progressive Podiatry Project link below.
Join the Research Round-Up
Free monthly newsletter, delivering the latest research straight to your inbox
Research Round-Up delivered at the end of each month


