Clarifying Therapeutic Movement - Avoiding Over & Under-Dosing our Rehab
Jan 10, 2023
When it comes to managing musculoskeletal pathologies clinicians can often take an all-or-nothing approach.
That is, everyone who walks in the door with a musculoskeletal pathology will receive an exercise program, or we have clinicians at the other end of the spectrum leaning on everything but exercise & movement-based therapies.
When we're staunchly sitting on one side of the fence we're often short-changing our results (and most importantly, our clients!).
In this article I want to share some clinical insights and actions we can take to help develop some nuance and improve our programming.
The first problem we need to address is defining what exercise & movement-based therapies are and how this looks clinically.
A trap that we can easily fall into, is thinking that a pathology needs a typical strengthening or gym exercise - eg: Eccentric Calf Raises for Achilles Tendinopathy, or High-Load Strengthening for Plantar Fasciopathy. Whilst yes, these are great rehab exercises, at times their prescription can actually cause more problems than they solve.
Exercise & movement-based therapy encompasses ALL types of movement - it's just our clinical reasoning and prescription of it that makes it mechanotherapy.
Mechanotherapy
“Therapeutic exercise is prescribed to promote the repair or remodelling of injured tissue”
Khan (2020)
All of these can be considered mechanotherapy (when we're prescribing to achieve a specific therapeutic goal)
- Walking 3 times per week for 20 minutes
- 4 sets of 25 single-leg calf raises
- 10 minute jogging warm up at 7:00min/km - 3 x 40m Strides - 20 minute run @6:00min/km pace with 3 x surges @4:45min/km pace at 5, 10, 15 minute mark - 10 min cool down.
Only one of these scenarios are what most clinicians will consider rehab, yet they all are...
How can we develop a more nuanced approach to prescribing exercise therapies & avoid swinging too far on the pendulum?

The Problem With The Pendulum
There's two very common scenarios we can see, one from either end of the pendulum.
The first problem occurs when we fall into the trap of thinking every musculoskeletal presentation needs a rehabilitation exercise.
Why this can create a problem is that for a portion of our clients we can potentially be overdosing their movement, further contributing to their pathology.
The second problem occurs when we err away from prescribing anyone anything. Instead we may simply recommend rest, or "just stop doing X activity", or relying on passive therapies to address symptoms without addressing the underlying problem - creating a perpetual treatment loop. Good for business, bad for client outcomes...
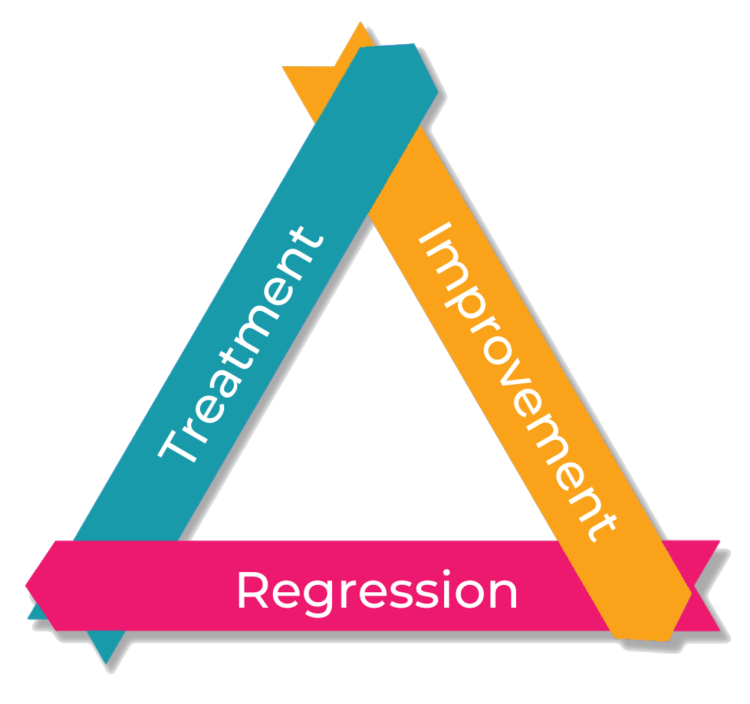
Treatment → Symptom Improve → Regression → Treatment → Symptom Improve etc...
Whilst there certainly is a role for passive therapies, I feel that when we're dealing with a pathology where the overall aim is/should be improving functional capacity, either physically &/or psychologically, their utilisation should be to open the Therapeutic Window, not to just address symptoms.
This can create a problem as we may be underdosing their movement, perpetuating their injury.
Clinically, if we have more in-depth discussions with our clients about what they are wanting from seeking out care, we can move beyond focusing on just treating their symptoms - as the symptom isn't often the real problem they're seeing us for!
ARTICLE: Ask Better Questions Gets Better Results - read it here
How Can We Know Which Way To Swing?
If we take a step back and think about the musculoskeletal presentation we are dealing with, ie: delve into our clinical history, it can quickly give us an idea of where we need to go.
It's relatively easy to address the pendulum from the 'no one gets exercise therapy' end of the spectrum, as we simply need to encourage movement.
The problem most clinicians experience is knowing what movement/exercises should we be encouraging & how much???
Clinical Scenarios
Scenario #1: Long-time runner, recently increased the frequency of their running from 3 days per week to 4 and over a period of 6-8 weeks developed some mid-portion Achilles symptoms. Chances are that this is more of a scenario where removing some of the running load then gradually re-introducing running loads may be all we need to do.
IF this approach doesn't work and a Capacity Gap remains, then we may introduce some exercise therapies to address the Capacity Gap.
ARTICLE: When LESS is MORE in Rehab read it here
Scenario #2: Relatively inactive individual, who has a desire to get back to walking. Tries to walk for an hour, Achilles flares, rests for a week until it feels better, walks again, flares again. Rinse & repeat. In this scenario it is a low-key version of the boom-bust cycle. The approach here would likely be introducing smaller bouts of activity at more regular intervals, then progressively working towards the client's desired 60 minute walk.
What some clinicians may not pick up on, is that even though no specific classic rehabilitation exercise has been prescribed, it is simply a movement prescription - this IS exercise therapies aka movement-based therapy aka rehab.
ARTICLE: The Importance of Therapeutic Movement for our Older Clients read it here
Scenario #3: Long-time runner with ongoing midportion Achilles tendon symptoms, slowly spiraling down into having less and less functional capacity. Has tried a myriad of passive therapies, orthomechanical interventions, footwear and the occasional slower re-introduction to running loads and just can't seem to get back to the mileage they're after - this history presents somewhat of a Capacity Gap as over time, despite the treatments, their capacity is diminishing - ie: could run 10km, then only 7km, then only 5km.
They're frustrated, distressed and feeling like they're never going to get back to running (it is actually quite rare that someone can't!)
This is a situation where we may engage in some prescribed exercises from the get go - to address physical AND psychological capacity (if someone is feeling like they can do less and less, this tends to be the focus - "I can't do XXX", let's get them focusing on what they can)
ARTICLE: Looking Beyond Physical Capacity read it here
Clinical Tips
Clinical History
- How long has the problem been presenting for?
The longer the problem, typically the higher the change prescribed exercises may come into play (not a blanket rule, but a general guidance of thumb) - What activities were they doing in the 8-12 weeks prior to your appointment?
Typically if something has changed addressing this change is the starting point. - Did anything load-related change? (footwear, surfaces, training intensity)
Approach as above in point 2. - What does their load distribution look like? (infrequent with large spikes, or very frequent with little down time)
Typically if it's more of a boom-bust scenario introducing lower dose-higher frequency is the go. In contrast, if it's high frequency-low recovery time it may simply be an increase in recovery time and a reduction in current load exposure. - Subjective Capacity Gap - What do they want to do vs what they can currently do?
Move beyond the symptom and get thinking functionally.
Clinical Assessment
- Clarification of a presenting Capacity Gap via functional testing. That is; if they can't do X activity, what regression of that movement can they do? If they can't run can they jog? If they can't jog can they hop? If they can't hop can they jump? If they can't jump can they do B/L calf raises at a fast tempo? etc etc...
I hope these tips are helping and as always, I'd love to hear your thoughts - comments or DMs are always welcome.
Also, early bird pricing for our 2 day workshop Functional Rehabilitation of Musculoskeletal Pathologies closes on the 28th March 2023.
Click here to find out more
Join the Research Round-Up
Free monthly newsletter, delivering the latest research straight to your inbox
Research Round-Up delivered at the end of each month

