Dosing Rehab WITHOUT Sets & Reps
Aug 07, 2023
There's a multitude of reasons when the typical sets & reps for exercise prescription may not be appropriate.
In recent articles & podcasts I've touched on AMRAP for TIME, today, we'll be doing a deeper dive into what it is, when we may utilise this option, and how we may program it (for rehab).
What Is AMRAP?
AMRAP - As Many Reps As Possible
This method sees a person complete as many repetitions of a given exercise or circuit of exercises, in a set period of time.
Background
AMRAP is more traditionally used in high-volume workouts in a strength & conditioning space (think crossfit).
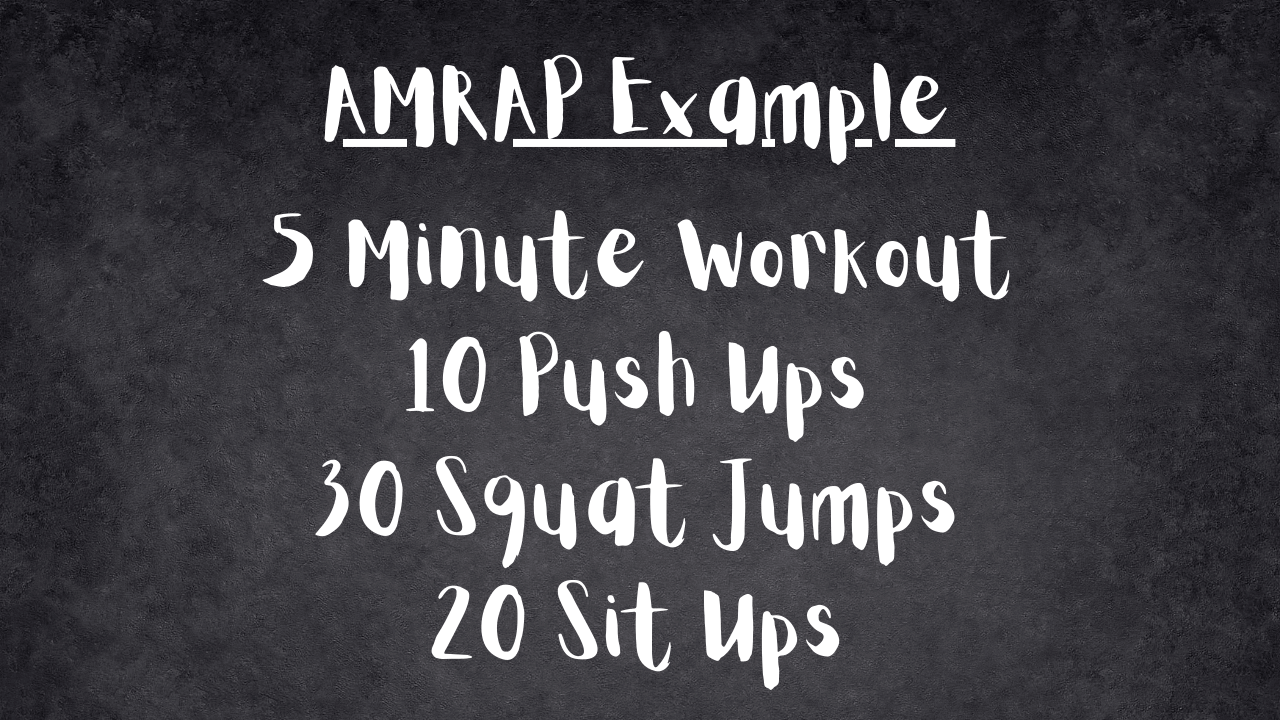
Now, AMRAP in torture boxes (aka crossfit gyms) will typically see a person perform continuos movements/exercises, without rest for a set period of time.
Performing AMRAP exercises will often deliver benefits for both strength, cardiovascular & metabolic health (if someone isn't pushed into rhabdomyolysis!).
However, due to the high workload and metabolic demands, a person may require more time between these types of workouts to allow of adequate recovery.
Is this type of workout suitable to someone in the early stages of injury or post-operative rehabilitation?
AMRAP in Rehab
There isn't a distinct line that exists where we see someone move from rehab mode to maintenance mode, or from rehab mode to performance mode, it's a gradual transition.
Rehab Mode
This is the phase of treatment where we may be dealing with higher degrees of reactivity (pain, inflammation, early-stage tissue repair & its subsequent mechano-sensitivity etc).
Typically we will be aiming for low-dose, high-frequency movement exposure.
This may be for a myriad of purposes, for example, early tissue remodelling &/or addressing movement-related fear/anxieties.
Maintenance Mode
Often when we have clients returning to their desired activities, whatever they may be, that don't have specific performance goals or aren't working towards further increasing capacity as they're back to doing what they love, maintenance mode commences.
Maintenance mode sees a person (hopefully) engage in long-term behaviours we've helped create, that will reduce the risk of re-injury or developing another injury in the future.
In some instances this may be creating a plan for long-term movement exposure to mitigate some risk factors that have contributed to their pathology. For example; a sedentary lifestyle in an older client who has been experiencing Achilles Tendinopathy, or a more sustainable approach to running via monitoring training loads in someone wh has been sufferring bouts of Plantar Fasciopathy with the occassional flare surge (that strangely aligns with their training spikes!).
Performance Mode
When we have facilitated a person moving along the continuum from rehab mode and they are looking to continue improving their relevant performance metrics.
That is, they have a specific goal in mind, requiring a specifically-dosed program.
For example; improving 10km race times, training for a marathon, or improving their relevant performance metrics relating to their chosen sport.
How quickly that transition occurs, not to mention how long someone stays in one mode will vary from person to person.

When we are in the early stage of rehabilitation our movement goals or prescribed movements may be quite specific (ie: isolated movements, set parameters for ROM), yet the highly reactive state of the tissue(s) can mean prescribing a definitive dose of sets & reps is playing roulette with the possibility of triggering a flare (ie: over-dosing our rehab), so our dosage may be somewhat general (with dosage parameters).
Depending on the severity of the injury or recovery time post-operatively, we can see tissues with a high degree of reactivity and a person regress to a lower level of overall physical conditioning. As they progress through the stages of rehabilitation we will often see their reactivity lessen, whilst their physical conditioning improves (ie: low reactivity | high conditioning).
Looking at this through the lens of a health practitioner prescribing rehabilitation exercises, it is in the early stages of rehabilitation where AMRAP for TIME can be very useful. It's also useful for conditioning, but more on that another time...
We know what we are wanting to prescribe;
eg: regular exposure to 1st MTPJ dorsiflexion/plantarflexion 2/52 post-operatively for a HAV correction procedure.

But the dosage will be incredibly varied given the varied responses & healing times of each individual patient.
In this example prescribing 3 x 20 repetitions to every person may be perfectly fine for many, but over-dose others.
Do Reps Really Matter in Rehab? - more here
By dosing the exercise AMRAP for TIME we can;
Encourage regular movement exposure.
In the early stages of healing we need mechanotransduction to be occurring, so our body knows what to put where, and how to orientate the tissues.
We deep-dive this in Exercise Therapies in Podiatric Practice
Therapeutic Movement & Dosing Rehab - more here
Alleviate some anxieties around the movement exposure &/or prescribed exercise.
Some people find the sets - reps - frequency etc confusing and overwhelming. The addition of a prescriptive program with lots of different numbers can add fuel to the fire, we want to do the opposite (more on this here).
Setting parameters for how to move (eg: tempo, range etc) and to simply to AMRAP in a set amount of time (30-60 seconds) can be a lot easier for people to digest.
Not to mention, that we are mitigating the risk of prescribed sets & reps over-dosing the tissue/area - which inevitably leads to less movement.
There are also a great number of clients we see that have movement-related fears (think catastrophising, the development of kinesiophobia etc) that may be driven by a number of things; previous experiences with health practitioners and movement prescription (ie: over-dosed or inappropriate rehab), a lower level of health literacy, not understanding what pain is and what it means (contextual factors etc).
For early tissue healing & overcoming some of these psychosomatic factors it's often the lower dose but higher exposure that's required for the physical &/or psychobehavioural responses to experience their positive effects.
Looking Beyond Physical Capacity - more here
Allow the movement exposure to ebb & flow with potential fluctuations in reactivity of the healing area.
The body is an immensely complex organsim, you're not the exception to the rule if you have a few days where it feels like you're either not making any progress or have taken 10 steps back.
Sleep, nutrition, stress, any number of factors will influence how our body responds to movement on any given day, especially when we are recovering from an injury or surgery.
By aligning our movement exposure to these fluctuations can allow us to help our clients navigate their rehabilitation in the presence of pain (more on this here).
Think of the Tortise & the Hare, consistency will often get you to the destination faster than surging forward then burning out.
Why Injuries NEED Movement - more here.

Getting Clients Onboard
When I discuss AMRAP for TIME in my workshops one of the most common questions regarding this is "How do you explain this to patients?".
When we're at the prescription part of the consultation I will have explained a number of things to my clients already.
- Their injury / surgery and a rough outline of the healing/recovery process.
- Framing expectations about timeframes, fluctuations in symptoms and progress.
- The role of movement in their healing & recovery (+/- the long-term role for maintenace &/or risk reduction).
I will then explain the importance of regaular low-dose movement as opposed to big bouts requiring long recovery periods (if we are in early stage rehab &/or have a highly-reactive tissue).
"Ok, so ___ times per day you're going to have your alarm set, when it goes off you're going to start the stopwatch and it will run for ___ seconds.
You're going to perform as many slow, controlled movements in this time as you can. The goal here is quality over quantity, I'd rather you do 7 movements that get to the right range of movement as opposed to knocking out 15 really fast, poor quality movements.
If you feel like it's getting a bit achey, you get a cramp, or just feel like you need a second to rest, take the time, but don't stop the clock.
Some times you'll get ___ within the 30 seconds, other times you might only get ___. It's not the number that's most important at this time, it's the consistency of doing the movement, because that's what's really working the magic."
Hopefully this has helped shed some light on a different approach to your movement prescriptions in a rehabilitation-sense.
Join the Research Round-Up
Free monthly newsletter, delivering the latest research straight to your inbox
Research Round-Up delivered at the end of each month

